AIDS denialists claim that HIV does not cause AIDS, that the risks of antiretrovirals outweigh their benefits or that there is not a serious HIV epidemic in sub-Saharan Africa. This webpage explains why these views are wrong.
We have deliberately kept the refutations of these myths on this page short. Instead of providing detailed scientific notes, we usually summarise key scientific findings and then provide links to more detailed refutations for readers who are interested. Additional material will be added to this site over time, to debunk other AIDS denialist myths. We recommend you monitor the site on a regular basis.
- HIV does not cause AIDS
- AIDS among minorities in the United States and other industrialised countries is caused by recreational drug use
- Studies, in particular one conducted by Nancy Padian and her colleagues, show that HIV cannot be transmitted heterosexually
- AIDS in haemophiliacs is caused by Factor VIII, a clotting agent in donated blood for haemophiliacs, not HIV
- AIDS in Africa is another name for old diseases caused by poverty
- There is no serious HIV epidemic in Africa
- AZT causes AIDS
- Although antiretrovirals work now, AZT when used as a monotherapy in the late 1980s and early 1990s killed more people than it helped
- The Concorde trial showed that AZT causes AIDS, or at least that AZT’s risks outweigh its benefits
- Antiretrovirals have not been tested in clinical trials
- Antiretrovirals taken by pregnant women are harmful to the foetus
- The Ugandan HIVNET 012 trial that studied the efficacy of single-dose nevirapine for mother-to-child HIV transmission prevention was scientifically and ethically flawed such that its results are unreliable
- HIV tests are unreliable and frequently produce false positives
- False positive HIV test results are likely in pregnant women
- Tests that measure HIV directly are meaningless because they only find dead virus particles
- AZT does not triphosphorylate and therefore cannot work
- HIV cannot be detected post-mortem
- HIV is an endogenous retrovirus
- HIV is a harmless passenger virus
- The fact that some HIV-positive people live in good health without treatment for many years proves that HIV is harmless
Myth #1: HIV does not cause AIDS
Fact: HIV has been shown beyond reasonable doubt to be the cause of AIDS.
There is an abundance of evidence showing HIV is the cause of AIDS. With very few exceptions, the human immunodeficiency virus itself or antibodies to HIV are detected in people with AIDS. Studies of people who are HIV-positive show they are more likely to develop AIDS symptoms and more likely to die at younger ages than people without HIV. Scientists can now describe in great detail how HIV infection occurs and causes AIDS. For detailed explanations see:
- NIAID: The Evidence that HIV Causes AIDS
- NIAID: The relationship between the Human Immunodeficiency Virus and the Acquired Immunodeficiency Syndrome
- Avert’s succinct and simple explanation of how we know that HIV causes AIDS
- TAC’s Magazine, Equal Treatment Issue 19, which explains the science of HIV
Also see:
These are two historically important papers that showed that HIV is the cause of AIDS. See this paper by Robert Gallo and Luc Montagnier. It describes how the discovery was made in the early 1980s.
Myth #2: AIDS among minorities in the United States and other industrialised countries is caused by recreational drug use
Fact: There is no evidence supporting the myth that AIDS in gay men and other minorities in the United States and other industrialised countries is caused by recreational drug use.
No published peer-reviewed study supports this theory. Alcohol use can disinhibit people so that they increase their risk of HIV infection (e.g. by not using condoms). Excessive alcohol use also increases the risk of people on highly active antiretroviral treatment (HAART) not adhering to their medication thereby leading to disease progression.
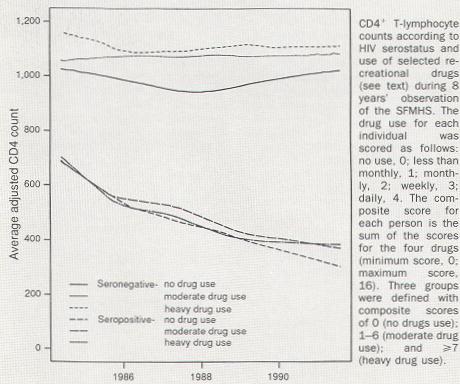
M.S. Ascher and team examined the drug use data of several research cohorts and found no correlation between drug use and AIDS. The graph below is from that study, Does drug use cause AIDS?, published in Nature in 1993.
As explained in an NIAID document:
Observational studies of HIV-infected individuals have found that drug use does not accelerate progression to AIDS (Kaslow et al., 1989; Coates et al., 1990; Lifson et al., 1990; Robertson et al., 1990). In a Dutch cohort of HIV-seropositive homosexual men, no significant differences in sexual behavior or use of cannabis, alcohol, tobacco, nitrite inhalants, LSD or amphetamines were found between men who remained asymptomatic for long periods and those who progressed to AIDS (Keet et al., 1994). Another study, of five cohorts of homosexual men for whom dates of seroconversion were well-documented, found no association between HIV disease progression and history of sexually transmitted diseases, number of sexual partners, use of AZT, alcohol, tobacco or recreational drugs (Veugelers et al., 1994).
A 2008 study, Recreational drug use and T lymphocyte subpopulations in HIV-uninfected and HIV-infected men, examined this issue in the MACS cohort. The conclusion was that there are “no clinically meaningful associations between use of marijuana, cocaine, poppers, or amphetamines and CD4 and CD8 T cell counts, percentages, or rates of change in either HIV-uninfected or HIV-infected men”.
Wild chimpanzees infected with the the immediate precursor to HIV-1 also have disease progression similar to HIV-1 infection in humans. Obviously recreational drug use cannot do this. See this article for further explanation.
Also see:
- Kaslow RA, Blackwelder WC, Ostrow DG, Yerg D, et al. No evidence for a role of alcohol or other psychoactive drugs in accelerating immunodeficiency in HIV-1-positive individuals. A report from the Multicenter AIDS Cohort Study. JAMA 1989;261(23):3424-9.
- Coates RA, Farewell VT, Raboud J, Read SE, et al. Cofactors of progression to acquired immunodeficiency syndrome in a cohort of male sexual contacts of men with human immunodeficiency virus disease. Am J Epidemiol 1990;132(4):717-22.
Myth #3: Studies, in particular one conducted by Nancy Padian and her colleagues, show that HIV cannot be transmitted heterosexually
Fact: Studies actually show the opposite, i.e. that HIV can be and is transmitted heterosexually.
Nancy Padian responds to this myth in detail in this article.
Myth #4: AIDS in haemophiliacs is caused by Factor VIII, a clotting agent in donated blood for haemophiliacs, not HIV
Fact: This has been disproved in numerous studies of haemophiliacs.
See Jon Cohen’s explanation in Science, written in 1994. The Factor VIII myth is based on the fact that a high proportion of haemophiliacs exposed to Factor VIII developed AIDS in the US. But the explanation is as follows: “[r]etrospective tests of the U.S. blood supply have shown that, in 1978, at least one batch of Factor VIII was contaminated with HIV” (NIAID document). The NIAID document further states:
- Among HIV-seronegative patients with hemophilia A enrolled in the Transfusion Safety Study, no significant differences in CD4+ T cell counts were noted between 79 patients with no or minimal factor treatment and 53 patients with the largest amount of lifetime treatments … ;
- In a report from the Multicenter Hemophilia Cohort Study, the mean CD4+ T cell counts among 161 HIV-seronegative hemophiliacs was 784/mm3;
- among 715 HIV-seropositive hemophiliacs, the mean CD4+ T cell count was 253/mm3 …;
- In another study, no instances of AIDS-defining illnesses were seen among 402 HIV-seronegative hemophiliacs treated with factor therapy or in 83 hemophiliacs who received no treatment subsequent to 1979 (Aledort et al., 1993; Mosely et al., 1993).;
- In addition to the evidence from the cohort studies cited above, it should be noted that 10 to 20 percent of wives and sex partners of male HIV-positive hemophiliacs in the United States are also HIV-infected… [This is, of course, due to heterosexual transmission of HIV from the index cases to their sex partners.]
Myth #5: AIDS in Africa is another name for old diseases caused by poverty
Fact: AIDS in Africa is characterised by recorded increases in the prevalence of a number of illnesses in young adults.
Numerous studies in Africa have shown that HIV infection predicts higher disease and death rates. While poor people have greater exposure to HIV and are more likely to progress to AIDS faster once infected with HIV, there is no evidence that poverty is the cause of AIDS. Here are two examples of the evidence that HIV is the cause of AIDS in Africa: A study in Rakai, Uganda disproves that poverty is the cause of AIDS. The study looked at nearly 20,000 people and found a much higher death rate among HIV+ people. Furthermore, the HIV-related death-rate was higher among better-educated and well-off people. A count of death certificates in South Africa from 1997 to 2002 showed a 57% rise in deaths that cannot be explained by population growth or improved death registration. While in 1997, most adults who died were between the ages of 60 to 79, by 2002 most adults who died were between the ages of 20 to 44 (see Statistics South Africa report on mortality). The report has since been updated for 2003 (and part of 2004). The HIV-related mortality trends have become even clearer. This cannot be explained by poverty, because (1) economic conditions in South Africa have not changed drastically enough to explain this sudden rise in adult mortality (on the contrary, the social wage in South Africa has increased during this time) and (2) if it had, we would expect to see a much higher rise in deaths among the elderly. The only plausible explanation of the increase in adult mortality in South Africa is HIV. (Also see South African Medical Research Council report). For many more examples related to Africa see:
- The Evidence that HIV Causes AIDS
- Equal Treatment Issue 19: Science of HIV (page 2)
- Rebuttal of Rian Malan
- A response to Rian Malan’s “last ever AIDS piece”
- Errors in Celia Farber’s article in Harper’s Magazine, March 2006
Myth #6: There is no serious HIV epidemic in Africa
Fact: The HIV epidemic is extremely serious in many sub-Saharan African countries.
This myth was perpetuated by Rian Malan in articles that appeared in the Spectator and Noseweek (a South African magazine) at the end of December 2003. For a list of studies showing high HIV prevalence in Africa, see the appendix to the Rebuttal of Rian Malan. Read the main text of the rebuttal of Malan for a detailed explanation of why his arguments are wrong. Also see this rebuttal of yet another Malan piece published in Noseweek in February 2007. Much more information confirming the seriousness of the HIV epidemic in many sub-Saharan African countries has been produced since the above rebuttal. Also see this Statistics South Africa report and this report by the South African Medical Research Council.
Myth #7: AZT causes AIDS
Fact: AZT and other antiretrovirals helps people with AIDS live longer.
In the first AZT trial on people with AIDS symptoms, known as BW 002, 19 patients out of 137 on placebo died and 1 patient out of 145 on AZT died. The AZT patients did better on a range of scores including quality of life (ref). In another randomized placebo-controlled study known as ACTG 016, the efficacy of AZT in reducing disease progression in symptomatic people with CD4 counts of 200 to 500 was again demonstrated. No benefit was found for people with CD4 counts above 500. (ref) Furthermore, numerous observational studies of AZT used in clinical practice have demonstrated its efficacy (ref). The myth that AZT causes AIDS is rebutted here in more detail. The table below shows how HAART (Highly Active Antiretrovial Therapy) has improved the probability of survival for people with HIV.
 Source: Survival of Persons with and without HIV Infection in Denmark, 1995–2005
Source: Survival of Persons with and without HIV Infection in Denmark, 1995–2005
Myth #8: Although antiretrovirals work now, AZT when used as a monotherapy in the late 1980s and early 1990s killed more people than it helped
Fact: Numerous studies have provided evidence that AZT used as a monotherapy in the late 1980s and 1990s prolonged lives.
PLEASE NOTE: OUR EXPLANATION SHOULD NOT BE READ AS AN ENDORSEMENT OF PROVIDING AZT AS A MONOTHERAPY. AZT SHOULD NOT BE USED AS A MONOTHERAPY EXCEPT IN SOME RESOURCE POOR FACILITIES FOR THE SOLE PURPOSE OF MOTHER-TO-CHILD TRANSMISSION PREVENTION AND WHERE SUCH FACILITIES CANNOT AFFORD TO PROVIDE BETTER OPTIONS.
This is a myth that is not only perpetuated by AIDS denialists. It is however unsupported by evidence and its perpetuation makes unnecessary concessions to denialists. In the late 1980s AZT monotherapy was of limited benefit and prescribed in doses that are now known to be too high and associated with more side-effects. Nevertheless, a number of studies demonstrated unequivocally that most patients who took AZT benefited. It is true that many people started AZT monotherapy too early and developed resistance. If they had delayed antiretroviral treatment until 1997 they would have had more treatment options, but this is a different issue that has no bearing on the question of whether people with HIV who took AZT monotherapy in the late 1980s and early 1990s did better or worse at the time than people at the same clinical stage of HIV who took nothing. NIAID’s article AZT and AIDS states:
Uncontrolled studies have found increased survival and/or reduced frequency of opportunistic infections in patients with HIV disease and AIDS who were treated with AZT or other anti-retrovirals (Creagh-Kirk et al., 1988; Moore et al., 1991a,b; Ragni et al., 1992; Schinaia et al., 1991; Koblin et al., 1992; Graham et al., 1991, 1992, 1993; Longini, 1993; Vella et al., 1992, 1994; Saah et al., 1994; Bacellar et al., 1994). In the Multicenter AIDS Cohort Study, for example, HIV-infected individuals treated with AZT had significantly reduced mortality and progression to AIDS for follow-up intervals of six, 12, 18 and 24 months compared to those not taking AZT, even after adjusting for health status, CD4+ T cell counts and PCP prophylaxis (Graham et al., 1991, 1992). In addition, several cohort studies show that life expectancy of individuals with AIDS has increased since the use of AZT became common in 1986-87.
Myth #9: The Concorde trial showed that AZT causes AIDS, or at least that AZT’s risks outweigh its benefits
Fact: The Concorde trial showed no such thing.
This misunderstanding of the Concorde trial is a popular myth amongst AIDS denialists. Nowadays, AZT treatment is not given by itself to people with HIV/AIDS. Three (or sometimes four) drugs are used, and AZT is often a component of the cocktail due to its efficacy. But in the late 1980s, AZT monotherapy was the only HIV medication available. AZT alone was not a very good drug; it was given in large doses (much larger than today) and resulted in numerous side-effects. Nevertheless clinical trials demonstrated unequivocally that it was much better than placebo for people with symptoms of AIDS and CD4 counts less than 500. In the first AZT trial on people with AIDS symptoms, known as BW 002, 19 patients out of 137 on placebo died and 1 patient out of 145 on AZT died. The AZT patients did better on a range of scores including quality of life.
In another randomized placebo-controlled study known as ACTG 016, the efficacy of AZT in reducing disease progression in symptomatic people with CD4 counts of 200 to 500 was again demonstrated. No benefit was found for people with CD4 counts above 500.
AIDS Denialists refer to the Concorde study as evidence for their belief that AZT’s risks outweigh its benefits. But the Concorde study did not show this.
The Concorde trial was the biggest AZT monotherapy study over the longest period of time. Its results actually show that AZT cannot be the cause of AIDS. Concorde only examined people with HIV without symptoms of AIDS. It compared two strategies: Approximately half the trial participants took AZT immediately and the other half took placebo until they developed AIDS.
Once patients progressed to AIDS, they were unblinded from the trial and given AZT. The participants taking AZT immediately had slower disease progression in the first year, but this dissipated with time resulting in no statistical difference in progression to AIDS. Since a large, approximately equal, number of participants in both arms progressed to AIDS, the trial demonstrated that AZT was no more harmful than placebo and therefore cannot be the cause of AIDS. (This was not the purpose of the trial incidentally, but it follows from its results.)
The denialists misunderstand the following about the Concorde trial: In a long-term follow up of the Concorde patients, those who deferred AZT treatment until they got AIDS were less likely (slightly, but statistically significantly) to die than those who took it immediately. But –and this is the critical– at this point the researchers were no longer comparing placebo against AZT.
As Brian Gazzard, one of the scientists involved in the Concorde trial, explained in an affidavit refuting an AIDS denialist initiated court case (the case was dismissed), Concorde was not testing whether AZT was better than placebo; this was already known. It was only trying to determine whether AZT should be taken before one developed AIDS symptoms. It concluded that one should not.
If the patients in the placebo arm stayed on placebo and never took AZT when they got AIDS, then a comparison would have been possible (and we can conclude from the trials described above that such hypothetical patients would have done very badly). But this is not what happened: patients on placebo indeed started AZT treatment when they developed AIDS because AZT had previously been shown to be beneficial for people with AIDS. If the patients who took AZT immediately had progressed to AIDS faster than the placebo group then one could conclude that AZT in patients without AIDS symptoms is dangerous. But the study simply did not show this. Read Brian Gazzard’s affidavit for a detailed explanation.
We now know why taking AZT as a monotherapy before developing symptoms of AIDS was an unsuccessful strategy. Patients taking one antiretroviral develop a strain of HIV resistant to the drug in a very short time (a few months on average). Consequently the drug stops destroying HIV and patients then experience the side-effects without the benefits. Then when they do eventually get AIDS, the drug no longer has a useful effect.
With today’s standard of triple-drug therapy, resistance takes, on average, several years to develop. When this happens, patients have to switch to a new antiretroviral cocktail. The current medical consensus is that treatment should still be deferred until a CD4 count of less than 350 or an AIDS-defining illnesses.
Myth #10: Antiretrovirals have not been tested in clinical trials
Fact: Every antiretroviral registered in South Africa and the United States as of July 2006 had been through a clinical trial which demonstrated its safety and efficacy.
We deal with this myth in detail on our page about the benefits of antiretroviral drugs.
Myth #11: Antiretrovirals taken by pregnant women are harmful to the foetus
Fact: The short-term evidence is unequivocal: Infants born to HIV-positive women who take antiretrovirals during pregnancy are much more likely to survive. While more long-term data is awaited, all the the available evidence shows that the reduced mortality conferred by antiretrovirals is sustained.
Children born to HIV-positive women are at much greater risk of dying than children born to HIV-negative women. The best available evidence shows that without antiretrovirals two or three out of every ten babies of HIV-positive women will contract HIV by the time they are born (i.e. excluding breastfeeding). With the best combination of antiretrovirals, this can be reduced to two or three in every 100 babies. A child who contracts HIV from his or her mother is at a much greater risk of dying than a child without HIV. Therefore it makes sense for a pregnant HIV-positive woman to take an antiretroviral combination to reduce the risk of her unborn infant contracting HIV.
See:
- Taha et al., The effect of human immunodeficiency virus infection on birthweight, and infant and child mortality in urban Malawi.
- Ryder et al., Mortality in HIV-1 seropositive women, their spouses and their newly born children during 36 months of follow-up in Kinshasa, Zaïre.
- Abrams et al., Neonatal predictors of infection status and early death among 332 infants at risk of HIV-1 infection monitored prospectively from birth. New York City Perinatal HIV Transmission Collaborative Study Group.
In 2007, the Cochrane Collaboration reviewed ARVs for pregnant women to reduce the risk of their babies contracting HIV. The review found eighteen high quality clinical trials that included over 14,000 pregnant women. The review states, “The trials compared the use of ARVs versus placebo, longer regimens versus shorter regimens using the same ARVs, and ARV regimens using different drugs and different durations of treatment.”
Its conclusion is unequivocal. It “found that short courses of certain ARV drugs are effective in reducing mother-to-child transmission of HIV, and are not associated with any safety concerns in the short term.”
So matters are clear for the short-term. What about long-term side-effects? This is a bit more complex. There are long-term concerns. The most serious of these is that there is evidence that ARVs damage the foetus’s mitochondria. Exactly what the consequences of this are we do not yet know. Some researchers suspect it might put these babies at higher risk of cancer. This has not been seen yet despite studies that have looked for it. But given that this intervention only started in the 1990s, it is too early to tell. Much more long-term data on children whose mothers took ARVs while they were pregnant are still needed. Nevertheless, the largest and best-conducted follow-ups so far reveal that very few of these children have suffered serious side-effects attributable to the drugs.
See:
- El Beitune et al., Antiretroviral therapy during pregnancy and early neonatal life.
- Benhammou et al., Incidence of cancer in children perinatally exposed to nucleoside reverse transcriptase inhibitors.
Consider that nearly half of all babies born with HIV die by the time they are three years old unless they get HAART. Consider also that even in an excellent health system in which HIV-positive children receive HAART from the day they are diagnosed at least 4% will die at a young age (see the CHER study), maybe much more than that. Finally, consider that so far very few serious clinical side effects have been seen in children born of mothers who took ARVs when they were pregnant. Taken together this makes the case for providing ARVs to pregnant women to reduce the risk of them passing the virus to their babies very compelling. Also, many pregnant HIV-positive women need HAART for their own health.
Myth #12: The Ugandan HIVNET 012 trial that studied the efficacy of single-dose nevirapine for mother-to-child HIV transmission prevention was scientifically and ethically flawed such that its results are unreliable
Fact: The HIVNET 012 trial, albeit imperfect from a book-keeping perspective, was a soundly conducted trial. There is no evidence that its scientific results are incorrect. The criticisms of the ethics of the trial made by AIDS denialists are without foundation.
This myth is extensively debunked elsewhere on the aidstruth.org website. See:
- Review of the HIVNET 012 Perinatal HIV Prevention Study
- HIVNET012: New Review Validates Findings
- Nevirapine Misinformation: Will It Kill?
- Reports on nevirapine threaten public health
- The HIVNET 012 Study
Myth #13: HIV tests are unreliable and frequently produce false positives
Fact: HIV tests for antibodies or the virus itself are highly reliable (both in terms of sensitivity and specificity).
There are two important measures when considering the accuracy of an HIV test or any screening or diagnostic test: sensitivity and specificity.
Sensitivity is a measure of how likely it is that the test will return positive results if the person being tested has HIV. A highly sensitive test is calibrated to capture every positive sample, but will probably produce some false positives because it is so sensitive that may react to other substances as well.
Specificity is a measure of how likely it is that the test will return negative results if the person being tested does not have HIV. A highly specific test will only react to the substance being tested for and exclude all true negatives, but it will also produce false negatives.
All medical screening and testing procedures—not just for those HIV but for cancers, for pregnancy, for diabetes, for Lyme disease, for everything—must balance sensitivity and specificity: it is inherent in the nature of testing. Ideally a test should have both high sensitivity and specificity. However, using two tests, one with high sensitivity and another with high specificity, is also fine and this is usually what is done with HIV.
HIV tests are calibrated to be extremely sensitive, in order not to miss any positive cases. This is because these tests are used to ensure that the blood supply is safe, and because it is important that people who are HIV-positive not be misdiagnosed as negative, because they will then not seek medical monitoring and treatment, and they may inadvertently spread the virus.
There are two categories of HIV tests: those that detect antibodies [ELISA and Western Blot tests) and those that detect the virus itself (viral load or PCR tests). It is the antibody tests that are usually used when people older than infants are first tested.
In the United States, the first step in HIV testing is usually the inexpensive ELISA screening test. The ELISA (Enzyme-Linked Immunosorbent Assay) can be used with blood or oral fluid (not saliva), and determines, with over 99.5% accuracy, if there are antibodies to HIV present. A rapid test produces results in less than half an hour; other test types require from several days to two weeks to get results. These tests are considered screening tests, not diagnostic tests: additional confirmatory testing is considered necessary to determine that an individual is HIV-infected. This is because the tests are so sensitive, they may in rare cases produce false positive or indeterminate results. Antibody tests are not accurate in people who have been infected with HIV very recently, because it typically takes 6 to 12 weeks, and can take as long as 6 months, to develop the antibodies to HIV that the test reacts to. People recently exposed to HIV should seek a PCR test to determine if they are in the stage known as “active infection.”
Most people in sub-Saharan Africa and other resource-poor settings are tested using rapid antibody tests that give results in 20 to 30 minutes. Occasionally these tests give indeterminate results. In those situations a blood sample from the person being tested is sent to a laboratory where a different test is carried out.. Different testing, screening and diagnostic protocols reflect the reality of economic and health services inequality, not ambiguity about the existence of HIV and its causative role in AIDS.
The following is a typical way in which HIV infection is identified in people older than infants in South Africa:
- First the Abbott Rapid Determine antibody test is performed. It has been evaluated as 100% sensitive and 99.4% specific. In other words it is not expected to give a false negative (except for in the window period of course), and it gives a false positive 6 in every 1,000 tests. (Assuming a person has a 50-50 chance of being HIV-positive.)
- If the Abbott test is negative, the patient is assumed to be negative. If it is positive, then a PMC First Response confirmatory test is done. This is also 100% sensitive, but 98.8% specific.
- If either of the above tests are indeterminate or contradict each other, then an ELISA test is performed in a laboratory. [1]
A list of common rapid HIV tests (as of 2003) and their accuracies is available on this page of the Centre for Disease Control (CDC).
The Western Blot test is considered the gold standard against which other HIV tests are evaluated. But it is important to understand that a person is not diagnosed HIV-positive on the basis of one test alone, even the Western Blot. Instead, a testing algorithm, involving at least two tests, is used to make a positive HIV diagnosis.
Infants born to women known to be HIV-positive are tested directly for the virus itself, not antibodies, because all newborns of HIV+ women carry their mothers’ antibodies. Women who do not know their HIV status may choose to have their babies tested for antibodies—if the results are positive, a follow-up PCR test can determine if the child is actually infected. Mothers of HIV antibody-positive children should seek additional testing and, if necessary, treatment. Even without treatment, about 2/3 of children born to HIV-positive mothers are not infected and will clear their mothers’ antibodies in 6 to 18 months; the other 1/3 will be infected, and will therefore develop antibodies of their own in response, just as adults do. Antiretroviral treatment and other interventions can reduce the HIV infection rate in babies of HIV-positive womenfrom about 25-30% to below 2%.
We know HIV testing is a valid, reliable procedure because AIDS almost never occurs in people who do not test positive for HIV antibodies or the virus itself. The sensitivities and specificities of the HIV tests on the CDC page linked above were determined by independent evaluations against multiple HIV-1 and HIV-2 subtypes.
To see how unusual it is for AIDS to be diagnosed in someone found to be HIV-negative, consider this 1993 study of US AIDS patients (which has a simpler explanation here). Of 230,179 people clinically diagnosed with AIDS, only 299 were HIV-negative. 172 of the 299 were then re-evaluated. Of these 299, 131 were actually found to be HIV-positive, and 34 died before their status could be verified. That leaves 168 unexplained cases, fewer than one in a thousand. So already more than 15 years ago, HIV tests were very accurate. [2]
HIV tests have become even better since then. This is from a 2005 review of HIV testing in the United States:
The use of repeatedly reactive enzyme immunoassay followed by confirmatory Western blot or immunofluorescent assay remains the standard method for diagnosing HIV-1 infection (44, 45). A large study of HIV testing in 752 U.S. laboratories reported a sensitivity of 99.7% and specificity of 98.5% for enzyme immunoassay (45), and studies in U.S. blood donors reported specificities of 99.8% and greater than 99.99% (46, 47). With confirmatory Western blot, the chance of a false-positive identification in a low-prevalence setting is about 1 in 250 000 (95% CI, 1 in 173 000 to 1 in 379 000) (48).
For more information about HIV testing and diagnosis, and responses to the misrepresentations of HIV testing made by HIV denialists, see AIDStruth’s critique of “The AIDS Trap.” [Coming soon]
Notes
1. Assuming this procedure is carried out correctly, the probability of a false positive diagnosis is 0.0006. In other words, only 6 in 10,000 people who are HIV-negative will be incorrectly diagnosed as HIV-positive. This is based on the estimate that 10.8% of South Africans over the age of two are HIV-positive, determined by the HSRC’s 2005 Household Survey and confirmed by the recently released 2008 one. In practice, people at risk of HIV are more likely to be tested and the risk of a false positive is even smaller than calculated here. By the standards of medical accuracy this is extremely high, much better than a pregnancy test for example. ^back^
2. In these rare cases of idiopathic CD4 lymphocytopenia (ICL), patients have reduced numbers of CD4+ T-lymphocytes, and some of the opportunistic infections associated with AIDS, including ICL cryptococcosis, molluscum and histoplasmosis. People with ICL usually have a good prognosis and stable, not falling, CD-4 counts. ^back^
Myth #14: False positive HIV test results are likely in pregnant women
Fact: If proper protocol is followed, the risk of a false positive HIV result is extremely small.
Even in low prevalence populations, false positives are rare if proper protocols are followed. The Centre for Disease Control’s Revised Recommendations for HIV Screening of Pregnant Women states: False-positive Western blot results (especially those with a majority of bands) are rare. For example, in a study that used a sensitive culture technique to test approximately 290,000 blood donors, no false-positive Western blot results were detected (75). In a study of the frequency of false-positive diagnoses among military applicants from a low-prevalence population (i.e., <1.5 infections/1,000 population), one false-positive result was detected among 135,187 persons tested (76). An HIV test should be considered positive only after screening and confirmatory tests are reactive. A confirmed positive test result indicates that a person has been infected with HIV. False-positive results when both screening and confirmatory tests are reactive are rare. However, the possibility of a mislabeled sample or laboratory error must be considered, especially for a client with no identifiable risk for HIV infection. HIV vaccine-induced antibodies may be detected by current tests and may cause a false-positive result (i.e., there is no HIV infection, only an immune response to the vaccine antigen). Persons whose test results are HIV-positive and who are identified as vaccine trial participants should be encouraged to contact or return to their trial site or an associated trial site for HIV counseling, testing, and referral (CTR) services.
Incorrect HIV test results occur primarily because of specimen-handling errors, laboratory errors, or failure to follow the recommended testing algorithm (76). However, patients might report incorrect test results because they misunderstood previous test results or misperceived that they were infected (77). Although these occurrences are rare, increased testing of pregnant women will result in additional indeterminate, false-positive, and incorrect results. Because of the significance of an HIV-positive test result, its impact on a woman’s reproductive decisions, and the resulting need to consider HIV therapeutic drugs for both a pregnant woman and her infant, previous guidelines have emphasized that HIV test results must be obtained and interpreted correctly. In some circumstances, correct interpretation might require consideration of not only additional testing but also the woman’s clinical condition and history of possible exposure to HIV. In recent years many HIV rapid tests that deliver results within 45 minutes have been developed. When two of these tests are used to measure HIV status they are very accurate (both sensitive and specific). In high HIV prevalence populations they provide an accurate and affordable means for pregnant women to determine their HIV status. See:
- Evaluation of rapid tests in pregnant women in Cameroon
- Evaluation of rapid tests in pregnant women in Côte d’Ivoire
- Review of evidence for screening pregnant women in the United States
Myth #15: Tests that measure HIV directly are meaningless because they only find dead virus particles
Fact: Viral load tests give an excellent indication of the amount of live virus in a person with HIV.
Studies show that viral load increases in most patients with HIV over time. Also, scientists as a matter of course can routinely take a sample of blood of a person with HIV and culture HIV from it in a laboratory. This would not be possible if the HIV in a person’s body was already dead. For a technical explanation, read the NIAID article Course of HIV infection. This editorial in Annals of Internal Medicine reflects on the importance of viral load tests in HIV treatment.
Myth #16: AZT does not triphosphorylate and therefore cannot work
Fact: AZT has been shown to work in clinical trials. There is evidence that AZT triphosphorylates.
This is an obscure myth perpetuated by the Perth Group of AIDS denialists. Triphosphorylation is a chemical process that must take place for AZT to work.
AZT has been proven to work in clinical trials as well as studies of cohorts in real-world settings. Whether the mechanism for how it works is or is not fully understood is therefore secondary. Nevertheless, there is evidence that AZT can indeed be triphosphorylated both from laboratory experiments and from studies of the human body. Triphosphorylation is a chemical process that AZT undergoes in order to stop HIV from reproducing.
A detailed explanation of the evidence that AZT triphosphorylates is contained in David Back’s affidavit in a South African court case (case: 1894/2001). Here is a very simple explanation based on Back’s affidavit:
HIV reproduces by entering CD4+ T-cells and then using the reproductive machinery of the cell to reproduce itself. When HIV enters the CD4 cell, it must convert its RNA to DNA (see pages 4 and 5 of Equal Treatment Issue 19 or the BBC for a detailed explanation). An enzyme called reverse transcriptase is key to this process. AZT works by interfering with the DNA chain produced by reverse transcriptase and stopping the chain from growing. Once this happens, the virus is unable to continue its reproduction process. AZT must be converted to what is known as its triphosphorylated form inside cells if it is to work. This triphosphorylated form is known as AZTTP. The action of the virus’s reverse transcriptase enzyme actually inserts AZTTP into the growing viral DNA being produced from the virus’s RNA. Once this happens, the viral DNA can grow no further and the viral reproduction process stops. Besides laboratory experiments that have demonstrated that AZT triphosphorylates, studies such as CHARM have detected triphosphorylated AZT in the human body.
Myth #17: HIV cannot be detected post-mortem
Fact: HIV can be detected post-mortem with a high degree of accuracy.
This is very important because deceased tissue donors need to be tested to ensure that tissue recipients are not infected with HIV. See:
Myth #18: HIV is an endogenous retrovirus
Fact: HIV has been shown to be exogenous throughout 20+ years of research.
An endogenous retrovirus is one whose genetic material has been incorporated into that of the host. This happens when the genome of the virus incorporates itself into the chromosome of the host’s sex cell (sperm or egg) – or its progenitor – and thus, upon fertilization becomes part of the normal genome found in every cell in the body of the host. Over time, the endogenous retroviral genome usually accumulates deleterious mutations rendering it incapable of productive infection. One myth used by denialists is that HIV is one of these endogenous retroviruses. However, several lines of evidence from the published scientific literature refute this claim, and prove that it is an exogenous virus, found only in CD4+ T-cells and a few other CD4+ cell types (such as macrophages) and not found in most other host cells.
Early evidence:
In the very first publication regarding the identification of HIV, Dr. Luc Montagnier described several experiments showing that HIV was exogenous. The controls used in his co-culture experiments, for example, did not produce a reverse transcriptase signal, only those cells exposed to infected patient lymphocytes. This indicates that the signal did not originate from the genome of the uninfected donor cells. The RT signal (and thus the virus) was able to be passed on to other uninfected lymphocyte cultures and resulted in a similar RT signal pattern. This passing on of the virus is another line of evidence that HIV is unlikely to be endogenous [1].
Southern Blots:
The southern blot is a method for probing for the presence of a specific DNA sequence within a DNA sample. In southern blot hybridization, a small segment of single-stranded DNA is hybridized to genomic DNA. There is nothing in the human genome that hybridizes at reasonable stringency levels (i.e. the specificity of the test) to probes made from HIV-1 or HIV-2 proviral genomes[2]. One study did find two very short sequences (192bp and ~30bp) with some similarity (<60% and 95% respectively) to parts of the HIV genome. However, these two sequences were detected only under very low stringency (low specificity) and no other sequences with similarity to HIV were found [3].
PCR:
In experiments using PCR (another method for detecting specific genetic sequences) in infected patients’ lymphocytes, PCR detects HIV in only a fraction of the infected donor’s T-Cells [4]. This alone is enough to demonstrate that HIV cannot be endogenous. An endogenous virus, by virtue of its past integration in host germ cells, would be detectable in all nucleated cells of the host. In other experiments, HIV DNA was found in the lymphocytes of patients but only very rarely in sperm cells [5]. The absence of HIV DNA from certain cell types in patients again refutes the idea that HIV is endogenous.
The Genome Projects:
The genome projects have been a valuable tool in the field of genetics and also refute the idea that HIV is endogenous. At the time this article was being written, only two examples existed in the scientific literature of endogenous lentiviruses in mammals: one in rabbits and one in lemurs [6][7]. All sequenced primate genomes (including several human genomes) show no endogenous lentiviral genomes.
Common Sense:
Some common sense combined with a brief look at infections would likewise indicate that HIV is not endogenous. If it were endogenous, sequences would be most similar between family members and most different between distantly related individuals. However, this is not the case. Europeans of non-West African descent have been identified with HIV-2 infection, despite HIV-2 being predominantly found in West Africa [8]. Conversely, many Africans have been infected by HIV-1. If one claims that HIV is endogenous, one therefore also claims that West Africans with HIV-2 infections are more closely related to non-West African Europeans with HIV-2 infection than they are to their HIV-1 infected countrymen. This is simply absurd.
References
1. Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS). Barré-Sinoussi F, Chermann JC, Rey F, Nugeyre MT, Chamaret S, Gruest J, Dauguet C, Axler-Blin C, Vézinet-Brun F, Rouzioux C, Rozenbaum W, Montagnier L. Science. 1983 May 20;220(4599):868-71. PMID: 6189183
2. Characterization of a continuous T-cell line susceptible to the cytopathic effects of the acquired immunodeficiency syndrome (AIDS)-associated retrovirus. Folks T, Benn S, Rabson A, Theodore T, Hoggan MD, Martin M, Lightfoote M, Sell K. Proc Natl Acad Sci U S A. 1985 Jul;82(13):4539-43. PMID: 2989831
3. Novel human endogenous sequences related to human immunodeficiency virus type 1. Horwitz MS, Boyce-Jacino MT, Faras AJ. J Virol. 1992 Apr;66(4):2170-9. PMID: 1548756
4. Sensitive detection of HIV DNA in T4 lymphocytes of infected individuals by polymerase chain reaction.
Hsia K, Spector SA; International Conference on AIDS. Int Conf AIDS. 1990 Jun 20-23; 6: 160
5. HIV-particles in spermatozoa of patients with AIDS and their transfer into the oocyte. Baccetti B, Benedetto A, Burrini AG, Collodel G, Ceccarini EC, Crisà N, Di Caro A, Estenoz M, Garbuglia AR, Massacesi A, et al. J Cell Biol. 1994 Nov;127(4):903-14. PMID: 7962075
6. Discovery and analysis of the first endogenous lentivirus. Aris Katzourakis, Michael Tristem, Oliver G. Pybus, and Robert J. Gifford Proc Natl Acad Sci U S A. 2007 April 10; 104(15): 6261–6265. PMCID: PMC1851024
7. Parallel Germline Infiltration of a Lentivirus in Two Malagasy Lemurs. Gilbert C, Maxfield DG, Goodman SM, Feschotte C, 2009 PLoS Genet 5(3): e1000425. doi:10.1371/journal.pgen.1000425
8. HIV-2 infection in 12 European residents : virus characteristics and disease progression. Van Der Ende M. E.; Schutten M.; Thaoi Duong LY; Gruters R. A.; Osterhaus A. D. M. E. AIDS ISSN 0269-9370 1996, vol. 10, no14, pp. 1649-1655 (23 ref.)
Myth #19: HIV is a harmless passenger virus
Fact: Studies in vitro, ex vivo and in vivo all support HIV’s ability to deplete CD4+ T-cells.
There are some denialists that argue that HIV does exist but that it is merely a harmless passenger virus and that no evidence exists to claim otherwise. In fact, there are thousands of studies that support the cytopathic properties of HIV. While some aspects of how HIV destroys cells that are not fully understood, that it does so it beyond doubt. This is not unique to HIV, of course, as the effects of many diseases are known despite the mechanisms not being completely elucidated. Some of what is known (and supporting evidence will be cited) is the documented here. Since there are literally thousands upon thousands of papers on HIV, a representative few are cited here. This is by no means an exhaustive list.
Evidence shows us that AIDS the CD4+ T-cell depletion is due to HIV. This can be observed 1) in vitro (in cell cultures), 2) ex vivo (in tissues removed from animal models or patients), and 3) in vivo both in animal models and in infected individuals.
Myth #20: The fact that some HIV-positive people live in good health without treatment for many years proves that HIV is harmless
Fact: A small percentage of people infected with HIV do live for many years without developing AIDS. They are often known as long-term non-progressors. But such individuals are rare: without proper medical care, including antiretroviral drugs when needed, most HIV-positive people will eventually develop AIDS.
As putative evidence that HIV is harmless, some HIV/AIDS denialists point to examples of HIV-infected people who survive for many years, even decades, without receiving antiretroviral treatment. HIV denialists often claim that these people survived because they avoided antiretroviral therapy, and that diet, exercise, nutritional supplements or herbal therapies, stress reduction, hypnosis, and other interventions prevent progression to AIDS. These claims are untrue and dangerous.
It is true that a small number of people, often known by doctors and researchers as long-term non-progressors (LTNP), can survive with HIV and without treatment for prolonged periods (over 20 years in exceptional cases). Unfortunately, without careful monitoring and treatment, most HIV-infected people will develop AIDS within ten years of infection. Those who live longer without standard medical care are not always in good health, and some HIV-infected AIDS denialists (e.g., Christine Maggiore) have died of AIDS-related conditions just months after claiming to be healthy. Ignoring HIV infection, avoiding properly qualified doctors, or hoping that a healthy lifestyle will prevent disease indefinitely, will result in the unnecessarily early illness and death of the great majority of HIV-infected people.
